An Infectious Disease Researcher Answers Questions About COVID-19
Department of Biology professor Shweta Bansal, head of the disease ecology and research lab at Georgetown, has created a list of answers to COVID-19 FAQs for our students, faculty and staff. Her research examines how social behavior and population structure shape infectious disease transmission and how knowledge of such processes can improve disease surveillance and control.
This virus sounds just like flu. Why is this a big deal?
There have been many comparisons between influenza and SARS-Cov-2, the virus that spreads COVID-19. But the truth is that the two infections are quite different:
- SARS-Cov-2 spreads more easily than flu;
- SARS-Cov-2 produces a high rate of asymptomatic (i.e. no symptoms) or mild infection which makes it challenging to track individuals who are infected and isolate them to prevent transmission;
- Since SARS-Cov-2 is a new virus, everyone in the human population is susceptible to it (i.e. no one has immunity or protection from being infected to it sometime in the past).
- SARS-Cov-2 has a high fatality rate, 10-20 times higher than flu.
These features allow the virus to spread easily, be undetected and affect everyone, making COVID-19 a dangerous epidemic. In addition, we don’t have a vaccine or antivirals for COVID-19, so social distancing and handwashing are our primary options for limiting transmission.
There is so much we don’t know about this virus. Shouldn’t we wait to act till we know more?
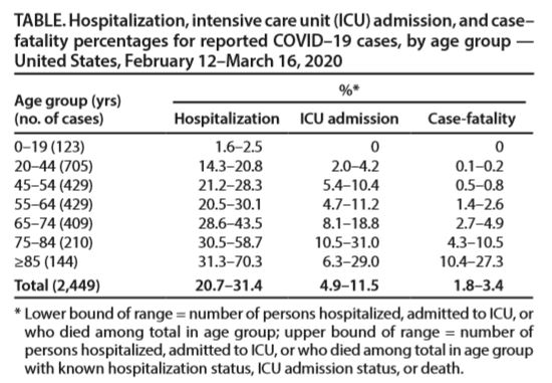
Is there a lot of uncertainty about this pathogen and outbreak? Yes, absolutely. But the data that we do have is more than enough to tell us that we must act NOW. The latest data from the CDC tells us that this disease is extremely risky for the US population, showing ~14-20% of individuals aged 20-44 (most of you) and ~30-45% of individuals aged 64-74 (most of our parents) need hospitalization after being infected. Those are sobering facts and are a call to action!
The full data is here (Data describe outcomes among those tested due to travel history or severe symptoms):
The virus doesn’t seem to affect young people very much. Can we have the at-risk population social distance and allow healthy, young people to be infected to create herd immunity?
This sounds like a good idea and might work if we were working with a simpler pathogen. In fact, the UK government was on track to implement this as a policy, but realized in enough time that it was a dangerous idea.
There are two issues that make this idea extremely risky:
- It’s not clear yet who is at-risk. There are many individuals that seem not at-risk (young, no comorbidities, etc) that are ending up in the ICU or dying from this virus (see data I mention above). We know age is certainly a risk factor, but there are likely a number of others such as genetic susceptibility, health behaviors (e.g. smoking) that make people high-risk.
- Isolating infected individuals once they are infected is challenging because many individuals are asymptomatic (show no symptoms) and because it appears that it’s possible to transmit before symptoms appear.
I have heard that there will be the same number of individuals that will be infected regardless of what we do now. Why should I bother social distancing if that’s the case?
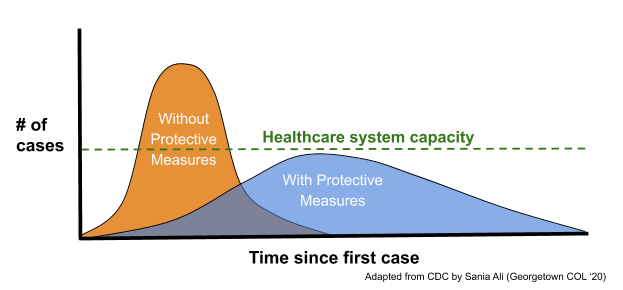
It may very well be true that we will have a large number of cases with social distancing. But with social distancing, we can spread the same number of cases over a longer period of time and our healthcare systems can keep up. Without social distancing, cases will continue at the present rate, ICUs and hospital beds will be overrun and hospitals will be short on supplies like masks and ventilators that health care workers need to keep themselves and us save. The graphic below illustrates this point:
What should I be doing to protect my family and help my community?
This outbreak is going to put a strain on all of us, so we must all do our part. Here are some suggestions:
- Remember the last time you had a bad cold/flu. Do everything you were doing then to keep your family/co-workers from getting sick.
- Wash your hands with soap and water for 20 seconds as many times as possible. (Might not be a bad idea to add a lotion chaser to keep those hands soft!)
- Work from home if you’re allowed to do so by your employer.
- Avoid all non-essential errands (everything but runs to the grocery store and pharmacy, and essential doctor’s visits).
- For the seniors in your family, avoid contact as much as possible; make sure they are stocked up on food and medications; set them up with tech for video calls.
- Make sure to keep in touch with friends and family through phone, chat, video calls (social distancing doesn’t have to mean social isolation).
- If you can support an essential worker living in your community (e.g. health care workers, cleaning staff, restaurant and grocery store workers, etc.) by cooking them a meal or helping them with household work, please consider helping.
- The above is more than enough to keep anyone very busy and contributing. But if you’d like to do even more, here is a list of suggestions.
Do face masks help against COVID-19? Should I stock up on them?
Studies show that face masks should be worn by those with COVID-19 to protect others around them. However, these face masks have not been shown to be particularly effective to protect uninfected individuals from infection (as they are difficult to wear correctly and consistently).
If you have face masks sitting around, save some in case anyone in the family gets sick. However, hospitals around the country will soon be experiencing a shortage on face masks and gloves. So, please don’t hoard these, and if you have a large supply accessible to you, consider donating these supplies to your local hospital. Protecting health care workers should be our first priority.
I have heard about medications such as hydroxychloroquine helping with COVID-19. Should I have my physician write a prescription so I can stock up on them?
There is reason to believe that a few existing drugs (such as hydroxychloroquine) may ameliorate the symptoms cause by COVID-19. However, no clinical trials reliably show that these work yet. Additionally, these medications are used regularly by individuals with chronic conditions (e.g. lupus) so please don’t take the drugs off the market and create a shortage for those who critically need them. Studies for the efficacy of these drugs for COVID-10 are ongoing, and hospitals around the world are providing them to patients with severe symptoms as needed.
I want to follow this epidemic more carefully. What are some reliable sources of information?
There is a ton of misinformation and myths about this public health crisis on the internet. I recommend the following resources for reliable information:
- NIH Coronavirus website
- WHO Coronavirus myths busted
- Hopkins Global Coronavirus Tracking
- Reliable coronavirus science journalism by Ed Yong and Helen Branswell
-by Shelby Roller (G’19)
- Tagged
- Announcement
- Biology