Georgetown Professor Discovers Key Findings to Stop Malarial Drug Resistance
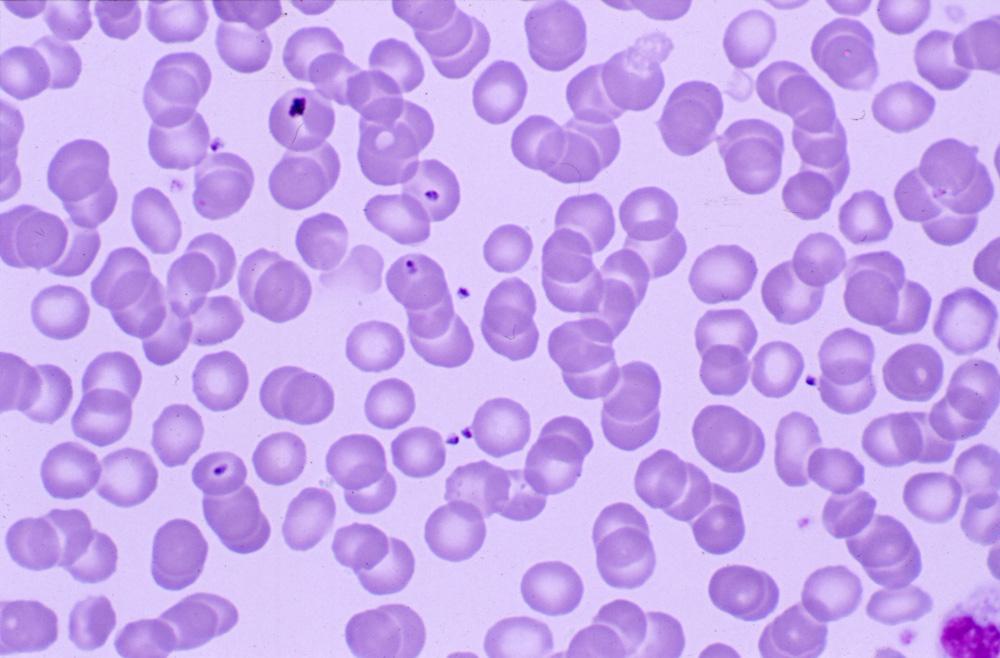
December 3, 2019 – Malarial disease infects millions of people every year. Until recently, drugs like chloroquine (CQ) and piperaquine (PPQ) have been effective against the parasite that causes it, Plasmodium falciparum. New widespread resistance to these drugs led Department of Chemistry professor Paul Roepe to research the mechanisms behind these new developments in an effort to stop the continued spread of the disease.
Knowing the Enemy
P. falciparum is the most dangerous species of the human malarial parasites, as it is accountable for almost every death from malaria. For the past five years, Roepe and his colleagues have been working collaboratively to understand the structure of the PfCRT transporter, a membrane protein that is a major determinant of drug resistance in malarial parasites.
“Proteins are not rocks, they are very dynamic,” says Roepe. “In this case this protein makes malarial parasites resistant to drugs. It binds and transports certain drugs across a membrane where the drugs are then rendered ineffective. We want to test this overall process with detailed atomic–level structural data.”
In their research recently published in Nature, Roepe worked with undergraduate and graduate students in addition to professors across universities. To begin, they used artificial pfcrt genes to make large amounts of PfCRT protein, which is essential for capturing its three-dimensional structure. This task alone took nearly twenty years to complete.
“Georgetown has the only lab to my knowledge that purifies all the different forms of this protein,” says Roepe. “The work that Hangbang Zhang and Ellen Howard in our group started back in 2000 to do this on the scale that is now possible was nothing short of heroic.”
Once the protein was purified, Roepe worked with Filippo Mancia, a professor at Columbia University, to capture the structure of PfCRT through cryo-electron microscopy and antigen-binding fragment technology. The lab is working now to combine this three-dimensional structure and their first-ever successful heterologous expression of a malarial parasite protein as described in their previous paper to further understand PfCRT function.
Roepe and his team are synthesizing this knowledge and finding strong evidence to suggest the location of mutations in PfCRT that contribute to CQ and PPQ drug resistance. Their research also suggests distinct mechanistic features that mediate resistance to CQ and PPQ. These data provide atomic-level insights into the molecular mechanism of this key determinant of antimalarial drug resistance.
Greater Implications
Approximately fifty percent of cases in Southeast Asia in which PPQ drugs were prescribed are not cured due to mutations in PfCRT. Previously, resistance to CQ drugs increased rapidly in the area, and appears to be related to PPQ resistance in unexpected ways. Roepe and his team are dedicated to continuing their research in the hopes of developing better drug therapy to counteract the effects of PfCRT mutations.
“Roughly 500 million people get malaria every year, and of those who die from the disease, most are children,” says Roepe. “Most of these deaths can be attributed to drug-resistant malaria. There are about 10 different malarial drugs currently in use, this protein is involved in resistance to half of them. We need to understand how this works to develop a therapy that kills drug-resistant malaria.”